What are viruses associated with respiratory infections?
"Viruses associated with respiratory infections" refer to the viruses that invade and proliferate in the epithelial cells of the respiratory tracts that could cause respiratory and systemic symptoms.
What are the common viruses associated with respiratory infections?
Viruses from the family Orthomyxoviridae (influenza viruses), the family Paramyxoviridae (paramyxoviruses, respiratory syncytial virus, measles virus, mumps virus, Hendra virus, Nipah virus and human metapneumovirus), the family Togaviridae (Rubella virus), the family Picornaviridae (rhinovirus), and the family Coronaviridae (SARS coronavirus) are the common respiratory viruses. In addition, adenoviru reovirus, coxsackie virus, ECHO virus, herpes virus, etc. can also cause infectious respiratory diseases.
What are coronaviruses?
Coronavirus are unsegmented single-stranded positive-strand RNA viruses. They belong to the order Nidovirales, the family Coronaviridae, and the subfamily Orthocoronavirinae, which is divided into α, β, γ, and δ genera according to their serotypic and genomic characteristics. Coronaviruses belong to the genus Coronavirus of the family Coronaviridae. It is named after the wreath-shaped protrusions on the envelope of the virus.
What are the shape and structure of coronaviruses?
Coronaviruses have an envelope encasing the RNA genome), and the virions (the whole viruses) are round or oval, often polymorphic, with a diameter of 50 to 200 nm. The novel coronavirus is 60 to 140 nm in diameter. The spike protein is located on the surface of the virus and forms a rod-like structure. As one of the main antigenic proteins of the virus, the spike protein is the main structure used for typing. The nucleocapsid protein encapsulates the viral genome and can be used as a diagnostic antigen.
How are coronaviruses classified?
Most coronaviruses infect animals. Currently, three types of coronaviruses have been isolated from humans: Human Coronaviruses 229E, OC43, and SARS coronavirus (SARS-CoV). There are 6 types of coronaviruses previously known to infect humans. 229E and NL63 (of alphacoronaviruses), OC43 (of betacoronaviruses), HKU1, Middle East Respiratory Syndrome Coronavirus (MERS-CoV), and Severe Acute Respiratory Syndrome Coronavirus (SARS-CoV).
Recently, a novel coronavirus was isolated from the lower respiratory tract of patients in “Wuhan, who were suffering from pneumonia due to unknown causes (The World Health Organization (WHO) called it 2019-nCoV while the International Committee on the Taxonomy of Viruses (ICTV) named it SARS-CoV-2. It was subsequently confirmed that the virus is capable of human-to-human transmission.
This novel coronavirus is very similar in terms of the genome sequences to six previously discovered coronaviruses. An analysis of their genetic sequence homology revealed that the new virus has many similarities with SARS-CoV. This novel coronavirus is now classified as a beta-coronavirus.
Which wild animals carry coronaviruses?
Many wild animals carry pathogens and are potential transmission vectors of certain contagious diseases. Bats, civets, badgers, bamboo rats, and wild camels, etc. are known hosts of coronaviruses.
The outbreak of novel coronavirus pneumonia originated in Wuhan has many similarities to the SARS outbreak in Guangdong back in 2003: both began in the winter; the initial cases were traced to contacts with fresh, live animals in a market; both were caused by a previously unknown coronavirus.
Due to the similarity of the genomic sequences between the novel coronavirus and a coronavirus found in bats, which is 85% or higher, it is speculated that bats are the natural hosts of the novel coronavirus. Like the SARS coronavirus that caused the “outbreak in 2003, the novel coronavirus is likely to have intermediate hosts between bats and humans yet unknown to us.
Therefore, one should refrain from consumption of uninspected wild animals or uncooked food such as meat sold by roadside sellers.
How do coronaviruses transmit from animals to humans?
Many coronaviruses that infect humans could be found in bats, which are natural reservoirs of coronaviruses. Bats are likely to be the original host of the novel coronavirus. Transmission from bats to humans might have occurred after mutation via an intermediate host(s). The genomic sequence analysis showed a more than 85% homology between the novel coronavirus and a coronavirus in bats. However, there are several other possible intermediate hosts between bats and humans, which have not been confirmed yet. Animal-to-human or human-to-human transmission relies mainly on two routes: contacts and droplets.
The coronaviruses that are currently known to cause pneumonia in humans include HKU1, SARS-CoV, MERS-CoV, and 2019-nCoV.
How resilient are coronaviruses in different environments?
Viruses generally can survive for several hours on smooth surfaces. If the temperature and humidity permit, they can survive for several days. The novel coronavirus is sensitive to ultraviolet rays and heat. Sustained heat at 132.8ºF for 30 minutes, ether, 75% alcohol, chlorine-containing disinfectants, peracetic acid, chloroform, and other lipid solvents can effectively inactivate the virus. Chlorhexidine (also known as chlorhexidine gluconate) also effectively inactivates the virus.
The survival time of the novel coronavirus 2019-nCoV at different environmental temperatures is as follows.

How virulent is the 2019-nCoV?
Common coronaviruses mainly infect adults or older children, causing the common cold. Some strains can cause diarrhea in adults. These viruses are mainly transmitted by droplets, and can also be spread via the fecal-oral route. The incidence of corona virus infection is prevalent in winter and spring. The incubation period for coronaviruses is usually 3 to 7 days.
2019-nCoV is a coronavirus that underwent antigenic mutations. The incubation period of the virus is as short as 1 day but generally considered to be no longer than 14 days. But it should be noted that some reported cases had an incubation period of up to 24 days.
To measure the degree of harm caused by a virus, both infectivity and lethality should be considered. The new coronavirus is highly-infectious and can be fatal, but its lethality has not been determined at present.
Can humans develop immunity to 2019-nCoV?
Scientific data on the level and the duration of protective immune antibodies produced in patients after infection of the novel coronavirus remain scarce. In general, the protective antibodies (immunoglobulin G, IgG) against a virus can be produced two weeks or so after an infection, and may exist for several weeks to many years, preventing re-infection of the same virus after recovery. Currently efforts are underway to test whether recently recovered from 2019-nCoV infection carry protective antibodies in the blood.
What is Severe Acute Respiratory Syndrome (SARS)?
Severe acute respiratory syndrome (SARS) is a disease caused by SARS-CoV. The main symptoms of SARS include fever, cough, headache, muscle pain, and other symptoms of respiratory infection. Most SARS patients recover with or without medical treatment. Its fatality rate is about 10%; those over 40 years of age or with underlying diseases (such as coronary heart disease, diabetes, asthma, and chronic lung diseases) are most at risk to develop the fatal disease.
What is Middle East Respiratory Syndrome (MERS)?
Middle East Respiratory Syndrome is caused by MERS-CoV. It was first reported in middle-eastern countries including Saudi Arabia, United Arab Emirates etc. People who are infected by MERS-CoV can develop acute respiratory distress syndrome (ARDS), while the most common manifestations being fever with tremors, coughing, shortness of breath, sore muscles and gastrointestinal symptoms such as diarrhea, nausea, vomiting or stomachache.
Severe cases are featured by respiratory failure which require mechanical ventilation and supportive treatment in ICU. Some patients developed organ failures, especially renal failure and sceptic shock which eventually led to death. The case fatality rate is about 40%. Since the onset of the first MERS case in September 2012 until May 2015, MERS cases have been reported in 25 countries around the world, posing a serious threat to public health.
What is novel coronavirus? Why has it become epidemic?
The newly discovered coronavirus is a mutated novel coronavirus (β genus), which is named 2019-nCoV by the WHO and SARS-CoV-2 by the ICTV. On January 10, 2020, genomic sequencing of the first sample of 2019-nCoV was completed, and the viral genomic sequences of five more samples were subsequently announced.
Due to the antigenic mutations that made this corona virus new to humans, the general population lacks immunity against the new strain. Furthermore, there are more than one routes of transmission for this virus. These factors resulted in the novel coronavirus becoming epidemic.
What is community-acquired pneumonia?
Community-acquired pneumonia (CAP) refers to infectious pulmonary parenchymal pneumonia (including in the alveolar wall, which belongs to the lung interstitium in a broad sense) contracted outside the hospital setting, including pneumonia from known pathogens presenting after admission within its average incubation period.
What are the diagnostic criteria for community-acquired pneumonia?
The diagnostic criteria for community-acquired pneumonia are:
- Onset in community.
- The clinical manifestations of pneumonia are as follows.
- New presentation of cough, sputum, or exacerbation of existing respiratory diseases, with or without purulent sputum/chest pain/dyspnea/hemoptysis.
- Fever.
- Pulmonary consolidation and/or presence of wet rales.
- WBC (white blood cells) counts higher than 10×109/L or lower than 4 × 109/L, with or without a left shift of neutrophil nucleus (a sign of immature neutrophils).
- Imaging characteristics. Radiographic examination revealing patchy infiltrates, lobular/segmental consolidation, or interstitial changes with or without pleural effusion.
If any items in (2) is positive and the imaging results support, a diagnosis of community-acquired pneumonia could be made after ruling out non-infectious diseases.
Which pathogens cause community-acquired pneumonia?
The most common pathogens that cause acute respiratory diseases include bacteria, viruses, or a combination of bacteria and virus. New pathogens, such as the novel coronavirus, can cause an epidemic or pandemic of an acute respiratory disease.
Bacteria are the main cause of community-acquired pneumonia. Streptococcus pneumonia is one of the most common bacterial pneumonia. Other bacterial pathogens include Mycoplasma, Chlamydia, Klebsiella pneumoniae, Escherichia coli, and Staphylococcus aureus; pneumonia caused by Pseudomonas aeruginosa and Acinetobacter baumannii have also been reported.
The virus detection rate for adult CAP patients in China is 15% to 34.9%, with influenza viruses including Haemophilus influenzae occupying the top spot. Other viral pathogens include parainfluenza virus, rhinovirus, adenovirus, human metapneumovirus, respiratory syncytial virus, and coronavirus. 5.8% to 65.7% of patients with positive virus test results are coinfected with bacteria or atypical pathogens.
How is community-acquired pneumonia transmitted?
Theoretically, all pathogens that cause community-acquired pneumonia have potential for human-to-human transmission. Routes of transmission from the source of infection to susceptible populations are droplet transmission, contact transmission, and airborne transmission.
Apart from the cold weather, the major factors such as movement of population (for example, the sizable migration during Spring Festival in China) makes winter more likely for respiratory infectious diseases to strike. It is mainly transmitted through droplets emitted by the patients or virus carriers when they cough or sneeze.
What are the risk factors for transmission of community-acquired pneumonia?
Autumn and winter are seasons prone to see the prevalence of respiratory viruses such as influenza, and various other respiratory infections may occur. This made it difficult to distinguish the early stage of COVID-19 from other upper respiratory infections.
The main sources of infection in community-acquired pneumonia include patients, their families, visitors, and their living environment.
The dissemination and outcomes of community-acquired pneumonia are associated with the following factors.
- Environmental conditions: air pollutants, overcrowding in confined spaces, humidity, indoor hygiene, seasons, and temperature.
- Accessibility and effectiveness of health care services and infection prevention measures: Accessibility and availability of vaccines and health care facilities, and isolation capabilities.
- Host factors: age, smoking habits, transmissibility, immune status, nutritional status, previous infection or co-infection of other pathogens, and overall health.
- Pathogen characteristics: routes of transmission, infectivity, virulence, and microbial population (inoculation size).
How to prevent community-acquired pneumonia?
Control the source of infection: When coughing or sneezing, the patient with acute respiratory diseases should cover their nose and mouth with the arm or other materials (handkerchiefs, paper towels, or masks) to reduce droplet transmission. After exposure to respiratory secretions, perform hand hygiene immediately, and wash hands frequently in daily life.
Personal precautions are as follows:
- Maintain a balanced diet, ensuring adequate nutrition, and maintaining oral health can help prevent against infection.
- Exercise regularly to boost immunity.
- Quit smoking, limit alcohol consumption, and stay in good spirits.
- Ensure indoor ventilation: natural ventilation and/or use of exhaust fans for better airflow.
- Get vaccinated if available.
Who are susceptible to 2019-nCoV?
“The novel coronavirus is newly emergent in humans. Therefore, the general population is susceptible because they lack immunity against it. 2019-nCoV can infect individuals with normal or compromised immunity. The amount of exposure to the virus also determines whether you get infected or not. If you are exposed to a large amount of virus, you may get sick even if your immune function is normal. For people with poor immune function, such as the elderly, pregnant women or people with liver or kidney dysfunction, the disease progresses relatively quickly and the symptoms are more severe.
The dominant factor determining whether one gets infected or not is the chance of exposure. So, it cannot be simply concluded that better immunity will lower one’s risk of being infected. Children have fewer chances of exposure and thus a lower probability of infection. However, at the same exposure, senior people, people with chronic diseases or compromised immunity are more likely to get infected.
What are the epidemiological characteristics of COVID-19?
The emergent epidemic of COVID-19 has experienced three stages: local outbreak, community communication, and widespread stage (epidemic).
Transmission dynamics: in the early stage of the epidemic, the average incubation period was 5.2 days; the doubling time of the epidemic was 7.4 days, i.e., the number of people infected doubled every 7.4 days; the average continuous interval (the average interval time of transmission from one person to another) was 7.5 days; the basic regeneration index (R0) was estimated to be 2.2-3.8, meaning that each patient infects 2.2-3.8 people on average.
Main average intervals: for mild cases, the average interval from onset to the initial hospital visit was 5.8 days, and that from onset to hospitalization 12.5 days; for severe cases, the average interval from onset to hospitalization was 7 days and that from onset to diagnosis 8 days; for fatality cases, the average interval from onset to diagnosis was significantly longer (9 days), and that from onset to death was 9.5 days.
Communication stages: The COVID-19 epidemic passed three stages: 1) the stage of local outbreak (cases of this stage are mostly related to the exposure of a seafood market); 2) the stage of community commu“nication (interpersonal communication and clustering transmission in communities and families); 3) widespread stage (rapid spread, with large population flow, to the entire country of China and even the world.)
What are the routes of transmission of 2019-nCoV?
At present, it is believed that transmission through respiratory droplets and contacts is the main routes, but there is a risk of fecal-oral transmission. Aerosol transmission, mother to child transmission and other routes are not confirmed yet.
- Respiratory droplets transmission: This is the main mode of direct contact transmission. The virus is transmitted through the droplets generated when patients are coughing, sneezing or talking, and susceptible persons may get infected after inhalation of the droplets.
- Indirect contact transmission: The virus can be transmitted through indirect contacts with an infected person. The droplets containing the virus are deposited on the surface of the object, which may be touched by the hand. The virus from the contaminated hand may get passed to the mucosa (or mucosae) of oral cavity, nose and eyes of the person and lead to infection.
- The live novel coronavirus has been detected from feces of confirmed patients, suggesting the possibility of fecal-oral transmission.
- Aerosol transmission: When the droplets are suspended in the air and lose water, pathogens left behind to form the core of the droplets (i.e. aerosols). Aerosols can fly to a distance, causing long-distance transmission. This mode of transmission is called aerosol transmission. There is no evidence that the novel coronavirus can be transmitted through aerosol yet.
- Mother to child transmission: A child of the mother with COVID-19 was confirmed to have positive throat swabs after 30 hours of birth. This suggests that the novel coronavirus may cause neonatal infection through mother to child transmission, but more scientific researches and evidence are in need to confirm this route.
What is droplet transmission?
A droplet generally refers to a water-containing particle with a diameter greater than 5 μm.
Droplets can enter mucosal surfaces within a certain distance (typically 1 m). Due to the relatively large size and weight of the droplets, they cannot stay suspended in the air for too long.
Generation of respiratory droplets:
- Coughing, sneezing or talking.
- During invasive respiratory tract procedures, such as suctioning or bronchoscopy, tracheal intubation, cough-stimulating movements including changing positions in bed or patting backs, and cardiopulmonary resuscitation, etc.
- Pathogens transmitted by droplets: influenza virus, SARS coronavirus, adenovirus, rhinovirus, mycoplasma, group A streptococcus and meningococcus (Neisseria), and recently discovered 2019-nCoV.
What is airborne transmission?
Airborne transmission is also known as aerosol transmission. Aerosols are suspensions of tiny particles or droplets that can be transmitted through the air. They are generally considered to be less than 5 μm in diameter, and the pathogens carried by them can still be infectious after traveling long distances. Airborne pathogens can also be transmitted through direct contact. The airborne pathogens are classified as follows.
- Through the airborne route only: Mycobacterium tuberculosis, Aspergillus.
- Through multiple routes, but mainly airborne: measles virus, varicella-zoster virus.
- Usually through other routes, but can also be transmitted through airborne only in special scenarios (like tracheal intubation/incision, open-airway suctioning and other aerosol-generating procedures): smallpox virus, SARS coronavirus, 2019-nCoV, Influenza virus and norovirus etc.
What is contact transmission?
Contact transmission refers to the transmission of pathogens through direct or indirect contact through fomites (pathogen-carrying objects).
- Direct contact. Pathogens are transmitted through direct mucosal or skin contact with an infected host.
- Blood or bloody fluids enter the body through mucous membranes or non-intact skins (mainly viruses).
- Transmission caused by contact with secretions containing certain pathogens, commonly for infections by bacteria, viruses, parasites etc.
- Indirect contact. Pathogens are transmitted through contaminated objects or people. Pathogens of intestinal infectious diseases are mostly transmitted through indirect contact.
- Other important pathogens transmitted through indirect contact: MRSA (benzoxazole/methicillin-resistant Staphylococcus aureus), VRE (vancomycin-resistant enterococcus), Clostridium difficile.
What is a close contact?
Close contacts refer to persons who have contact with a patient who is confirmed or suspected with infection of 2019-nCoV), including the following situations.
- Those who live, study, work or have other forms of a close contact with a patient.
- Medical personnel, family members or others who have had a close contact with a patient without taking effective protective measures during diagnosing, treatment, nursing and visiting.
- Other patients and their accompanying people sharing the same ward with an infected patient.
- Those who shared the same transportation or elevator with the patient.
- Those who are deemed as such through on-the-spot investigations.
Why should close contacts be put under isolated medical observation for 14 days?
Currently the longest incubation period observed for 2019-nCoV is generally 14 days.
Strict monitoring of close contacts and other preventive measures are necessary. This is not only a socially responsible practice for the public health and safety but also consistent with the international convention. With reference to the incubation periods of diseases caused by other coronaviruses, the information from the recent cases of 2019-nCoV, and the current prevention and control practices, close contacts should be placed under medical observation for 14 days at home.
What are the clinical manifestations of COVID-19?
The onset of COVID-19 is mainly manifested as fever, but some early patients may not have fever, with only chills and respiratory symptoms, which can occur together with mild dry cough, fatigue, poor breathing, diarrhea etc. However, runny nose, sputum and other symptoms are rare. Patients may gradually develop dyspnea. In severe cases, the disease can progress rapidly, causing acute respiratory distress syndrome, septic shock, irreversible metabolic acidosis, and coagulation disorders in just a matter of days. Some patients start out with mild symptoms without fever. The majority of patients have a good prognosis, while a few become critically and sometimes fatally ill.
Do you know something on laboratory testing for COVID-19?
2019-nCoV can be identified by real-time reverse transcription polymerase chain reaction (rRT-PCR). For each case, specimens to be tested should be from lower respiratory tracts, such as bronchial/alveolar lavage fluid and deep sputum. Also, serum samples should be collected both at the onset of symptoms and after 14 days.
In the early stages of the disease, the white blood cell count stays normal or lower, but the lymphocyte count is decreased. While some patients have elevated liver enzymes, muscle enzymes, and myoglobin, most patients have elevated C-reactive protein and erythrocyte sedimentation rate. The procalcitonin levels stay normal and D-dimer is elevated in severe cases.
What are the characteristics of COVID-19 chest films?
In the early stages, chest films feature multiple small patchy shadows and interstitial changes, especially in the peripheral third of the chest, which then progress to bilateral ground glass opacities and pulmonary infiltrates. In severe cases, pulmonary consolidations and even “white-out” of the lungs are seen. Pleural effusions are rare.
How to identify COVID-19 cases clinically?
Persons who meet both the following conditions are considered suspected cases.
- Epidemiological history. The case has a travel or residence history in the epidemic areas within two weeks of the onset, or had a contact(s) with patients from the epidemic areas within 14 days of the onset, or other patients with fever and respiratory symptoms in the communities with reported cases or clustered outbreak.
- Clinical features. The most common symptom is fever. Some patients may not present with fever, but only chills and respiratory symptoms. Chest films show characteristics of viral pneumonia. During the early stage of the disease, white blood cell count is normal or below normal, while lymphocyte count may decrease.
How to confirm COVID-19 cases?
Once a case is identified as a suspected case, a positive result for 2019-nCoV nucleic acid on rRT-PCR testing of specimens (sputum, throat swabs, lower respiratory tract secretions etc.) or highly homologous sequences to the known novel coronavirus found after gene sequencing of the virus from a patient can confirm the diagnosis.
How to diagnose severe COVID-19 cases?
Severe cases refer to patients with unstable vital signs and rapid disease progression, with dysfunction or even failures of more than two organ systems. The progression of the disease may endanger the lives of patients.
What is the difference between COVID-19 and other pneumonia?
- Bacterial pneumonia. Common symptoms include coughing, coughing up sputum, or exacerbation of the original respiratory symptoms, with purulent or bloody sputum, with or without chest pain. It is generally not considered a contagious disease.
- SARS/MERS. Although the novel coronavirus is in the same family as SARS and MERS coronaviruses, a genetic evolution analysis shows that it belongs to a different branch of the same subgroup. It is neither a SARS nor a MERS virus, based on the viral genomic sequences. Due to the similarities between COVID-19-and SARS/MERS-caused pneumonia, it is challenging to distinguish them with clinical manifestations and imaging results. Therefore, a pathogen identification test by rRT-PCR is needed.
- Other viral pneumonia. Pneumonia caused by influenza virus, rhinovirus, adenovirus, human metapneumovirus, respiratory syncytial virus and other coronaviruses.
What should close contacts do with notice from Center of Disease Control?
Please follow the self-monitoring instructions and stay at home. Don’t panic. Don’t go to work. Don’t go out too often. Perform daily checks of health condition and report the records to the authority, and follow up with your community doctors regularly. If fever, cough or other symptoms appear, please go to community health centers for further evaluation and treatment.
What should I do if I am possibly infected with COVID-19?
Promptly go to the local designated medical institution for evaluation, diagnosis and treatment. When a seeking medical attention for a possible infection of 2019-nCoV, you should inform your doctor about your recent travel and residence history, especially if you’ve been to the epidemic areas recently, and any history of contact with pneumonia patients or suspected 2019-nCoV cases, and animals. It is extra important to note that surgical masks should be worn throughout the visit to protect yourself and others.
How to choose a medical institution for treatment?
Isolation and treatment should be performed in a hospital with proper conditions for isolation and protection. Critical cases should be admitted to an ICU as soon as possible.
What should be done if a patient requires transportation?
Patients should be transported in designated vehicles that are regularly disinfected and manned with well protected personnel.
Are there any drugs or vaccines against COVID-19?
At present, there are no specific antiviral treatments against COVID-19. Patients generally receive supportive care to relieve symptoms. Avoid irresponsible or inappropriate antimicrobial treatment, especially in combination with broad-spectrum antimicrobials.
There is currently no vaccine against the new disease. Developing a new vaccine may take a while.
How to treat COVID-19?
- Put patients to bed rest, provide with supportive care, maintain good hydration and electrolyte balance, internal homeostatis, and closely monitor vital signs and oxygen saturation.
- Monitor routine blood and urine test results, C-reactive protein (CRP), biochemical indicators (liver enzyme, myocardial enzyme, renal function, etc.), and coagulation function accordingly. Perform an arterial blood gas analysis when needed, and regularly review chest X-ray images.
- According to the changes in oxygen saturation, provide a timely effective oxygen therapy, including nasal catheter, oxygen mask, transnasal high-flow oxygen therapy, and noninvasive or invasive mechanical ventilation, etc.
- Antiviral therapy: There are currently no antiviral drugs with good efficacy.
- Apply antibacterial drug treatment: strengthen bacteriological monitoring, and start antibacterial treatment when there is evidence of secondary bacterial infection.
- Traditional Chinese medicine treatment. Treat according to the syndrome.
What are the clinical criteria for quarantine release and discharge?
- The condition of the patient is stable and fever has subsided.
- Lung imaging shows a significant improvement with no sign of organ dysfunction.
- The patient has had stable breathing, clear consciousness, unimpaired speech, normal diet and body temperature for more than 3 days. Respiratory symptoms have improved significantly, and two consecutive tests for respiratory pathogenic nucleic acid have been negative (at least one day in-between tests).
How to prevent respiratory infections in spring and winter?
Wash hands frequently with plain or antimicrobial soap and rinse with running water. Be sure to dry hands with clean towels. Wash hands immediately after contact with respiratory secretions (for example after sneezing).
Practice good respiratory hygiene/cough practices. Cover mouth and nose while coughing/sneezing with tissue, towel etc. and avoid touching eyes, nose or mouth afterwards before thoroughly washing hands.
Strengthen overall health and immunity. Keep a balanced diet, get enough sleep and regular exercise, and also avoid overworking.
Maintain good hygiene and proper ventilation. Open windows regularly throughout the day to let in fresh air.
Avoid crowded places or contact with persons with respiratory infections.
Seek a medical attention if fever, cough, sneezing, runny nose or other respiratory symptoms appear.
Why does flu caused by viruses become pandemic?
Influenza is mainly transmitted through respiratory droplets and contact from infected to susceptible people, or through contact with contaminated items. In general, its incidence peaks in autumn and winter. Human influenza is mainly caused by influenza A virus and influenza B virus. Influenza A viruses often undergo antigen mutations and can be further classified into subtypes such as H1N1, H3N2, H5N1, and H7N9. When new influenza virus subtypes appear, they easily become a pandemic because the population generally lacks immunity against them.
How to keep yourself away from the novel coronavirus?
- 2019-nCoV is mainly transmitted by droplets and contacts, therefore medical surgical masks must be worn properly.
- When sneezing or coughing, do not cover nose and mouth with bare hands but use a tissue or a mask instead.
- Wash hands properly and frequently. Even if there are viruses present on hands, washing hands can block the viruses from entering respiratory tract through nose or mouth.
- Boost your immunity, and avoid going to crowded and enclosed places. Exercise more and have a regular sleep schedule. Boosting your immunity is the most important way to avoid being infected.
- Be sure to wear the mask always! Just in case you come in contact with an infected person, wearing a mask can prevent you from inhaling virus-carrying droplets directly.
Can a mask block such small coronaviruses?
The masks are effective. Because the purpose of wearing the mask is to block the ‘carrier’ by which the virus is transmitted, rather than directly blocking the viruses. Common routes for transmission of respiratory viruses include close contact over a short distance and aerosol transmission over a long distance. Aerosols which people usually come in contact with refer to respiratory droplets from patients. Wearing a mask properly can effectively block respiratory droplets and therefore prevent the virus from directly entering the body.
Please be reminded that it is not necessary to wear a KN95 or N95 respirator. Regular surgical masks can block most virus carrying droplets from entering the respiratory tract.
What are the features of masks for different purposes?
Major types of masks: N95/KN95 respirators, surgical face masks, and cotton face masks.
N95/KN95 respirators can filter 95% of particles with an aerodynamic diameter greater than or equal to 0.3 μm, and block viruses. They can help prevent airborne diseases.
Disposable surgical face masks have 3 layers. The outer layer is hydrophobic non-woven layer which prevents droplets from entering the mask; the middle layer has a filter to block 90% of particles with a diameter greater than 5μm; and the inner layer in contact with the nose and mouth absorbs moisture. They are typically for sterile medical operations and be used to prevent airborne diseases.
Cotton face masks are heavy, stuffy, and do not fit closely to the face, and thus not effective against viruses.
Any difference between KN95 respirator and N95 respirator?
Respirators are a kind of respiratory protective gear. It’s designed to more closely fit on the face than regular masks, and effectively filter particles in the air. “N” indicates “non-oil-based uses” and a N95 mask can be used to protect against non-oil-based suspended particles; “95” means that the filtration efficiency is no less than 95%, indicating that this respirator, as proved by careful testing, can block at least 95% of very small (0.3 μm in size) tested particles.
If worn correctly, N95’s filtration efficiency is superior to regular and surgical masks. However, even if you wear it as required, it does not 100% eliminate the risks of infection.
KN95 is one of the ratings specified in the Chinese standard (GB 2626—2006) while N95 is one of the ratings specified in the American standard (42 CFR 84). The technical requirements and testing methods of these two ratings are basically the same, and they both have a filtration efficiency of 95% by their respective standards.
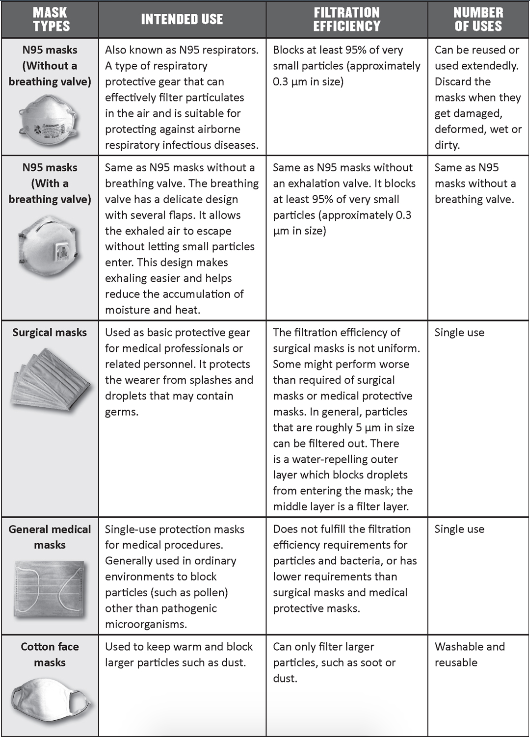
How to choose a mask?
The capability of masks to protect a wearer is ranked as follows: N95 respirators > surgical face masks > general medical masks > cotton masks.
N95 respirators come in two types, with or without breathing valves. While N95 respirators may make breathing more difficult for people with chronic respiratory diseases, heart disease, or other diseases with breathing difficulty, N95 respirators with breathing valves can make breathing easier and help reduce heat build-up.
N95 respirators with or without breathing valves have the same protection capability for the wearer. However, N95 respirators with breathing valves cannot protect people nearby an infected wearer. Therefore, carriers of the virus should wear N95 respirators without breathing valves to prevent spreading the virus. To keep the sterility of an environment, N95 respirators with breathing valves are not suggested because the wearer may exhale bacteria or viruses.
How to put on, use and take off a mask?
- After identifying the front, back, top, and bottom of the mask, wash your hands before wearing it. Make sure that the mask covers your nose and mouth, fits closely around the face to form a closed environment, so air passes through the mask, but not the gaps around it. Then, place the ear loops around each the ears.
- Besides the front and back side, the surgical mask also has a stiff bendable strip on top. When wearing it, with the front side facing outwards, you also need to make sure the stiff bendable strip is on top, molded around the nose.
- Wash hands thoroughly before taking off your mask. Push the front side of mask with one hand while holding the ear loops and remove them from around each ear with the other. Fold the mask with the back side in. If the back side is not contaminated, a limited reuse is allowed.
How often should a mask be replaced? Can N95 respirators be extendedly used or reused?
All masks have a limited protective effect and need to be replaced regularly in the following cases:
- when it is difficult to breath though the mask;
- when the mask is damaged;
- when the mask cannot fit snugly to the contour of the face;
- when the mask is contaminated with blood or respiratory droplets etc.;
- after contact with, or exit from, an isolation ward of any patient infected with an infectious disease requiring contact precautions (the mask has been contaminated).
At present, international organizations including the World Health Organization, have no definitive guidelines as to the optimal wearing time of N95 respirators. China has not yet introduced the relevant guidelines regarding the time of use of masks, either. Researches on the protective capability and wearing time of N95 respirators show that the filtration capability stays at 95% or above after 2 days of use, while the respiratory impedance has not changed much; the filtration capability is reduced to 94.7% after 3 days of use. The U.S. Centers for Disease Control and Prevention recommends that when N95 respirators are in short supply, N95 respirators can be extendedly used or reused unless they are visibly dirty or damaged (such as creased or torn).
How to keep my glasses from fogging up with a mask on?
To prevent glasses from fogging up while wearing a mask, please wash your hands before touching the mask, make sure the mask is worn in a correct orientation, make sure it fits your face snugly to form a closed environment allowing air to pass through the mask instead of the gaps around it.
How should special populations choose a mask?
- Pregnant women should choose masks they find comfortable for them. It is suggested that pregnant women consult with doctors for professional instructions on wearing masks.
- The elderly and patients with chronic diseases should ask for professional instructions on wearing masks because the body conditions of these people vary. For example, patients with heart and lung diseases may feel uncomfortable when wearing a mask, and it may even aggravate their illnesses.
- Generally, children’s face is small, so it is recommended that children wear masks specially made for the underaged by reputable manufacturers.
Why is handwashing important in preventing respiratory diseases?
The hands are the key medium in transmission of viruses that are transmitted through water, food, blood or blood products, respiratory droplets, digestive tract, in addition to direct or indirect touching. Studies show that proper handwashing is one of the most effective measures to prevent diarrhea and respiratory infections.
How to wash hands correctly?
Step 1: Apply soap to hands and scrub palm to palm with fingers interlaced.
Step 2: Put one palm on the back of another hand and scrub your fingers. Change hands.
Step 3: Scrub between your fingers.
Step 4: Rub the back of your fingers against your palms. Do the same with the other hand.
Step 5: Scrub your thumb using the other hand. Do the same with the other thumb.
Step 6: Rub the tips of your fingers on the palm of the other hand.
Step 7: Rub the wrist of one hand with the other hand while rotating it. Do the same with the other hand.
In each of the above steps, do each step no fewer than 5 times, and finally rinse your hands under running water.
What are the key moments for hand hygiene in daily life?
- When you cover a cough or a sneeze with your hand.
- After caring for a patient.
- Before, during, and after preparing food.
- Before eating.
- After going to the toilet.
- After touching animals.
- After touching elevator buttons and door handles or knobs.
- After coming home from outside.
How to clean hands if clean water is not available?
You can clean your hands with an alcohol-based hand sanitizer. Coronaviruses are not resistant to acid or alkali but are sensitive to organic solvents and disinfectants. 75% alcohol can inactivate the virus, so alcohol-containing disinfection products of an absolute (100%) concentration can be used as an alternative to washing hands with soap and running water.
Does handwashing with soap and clean water work against coronaviruses?
Yes, it does. Frequent hand washing is one of the effective measures to prevent viral infection such as rhinovirus and coronavirus. Rubbing hands with soap and water can effectively remove dirt and microorganisms on the skin, and rinsing out the soap under running water can also relieve irritation to the skin. Therefore, authoritative organizations such as the Chinese Center for Disease Control and Prevention, the World Health Organization, and the United States Centers for Disease Control and Prevention all recommend washing hands thoroughly with soap and running water.
Can 75% alcohol reduce risk of 2019-nCoV infection?
Yes. Coronaviruses are sensitive to organic solvents and disinfectants. 75% alcohol, chloroform, formaldehyde, chlorine-containing disinfectants, peracetic acid, and ultraviolet rays can inactivate the virus, so wiping hands and mobile phones with alcohol can prevent COVID-19 infection.
How to take care of the COVID-19 patient at home?
- Quarantine the patient from the rest of the family members and maintain a distance of at least one meter.
- Wear a mask when looking after the patient. Discard the mask after each use.
- Wash hands thoroughly with soap after having contact with the patient. The patient’s living space should be well ventilated.
Is it necessary for suspected cases with mild symptoms to be quarantined at home?
Yes. In case of insufficient treatment capacity and medical resources, The World Health Organization recommends that patients with mild symptoms (low-grade fever, coughing, sneezing, and asymptomatic sore throat) and no chronic diseases (such as lung diseases, heart diseases, kidney failure, or immune diseases) could be quarantined at home.
Notes:
- During the quarantine at home, patient needs to keep in touch with medical professionals until a full recovery.
- Medical professionals must monitor the development of symptoms to assess the patient’s condition.
- Patients and family members should maintain good hygiene and receive health care, prevention instructions and monitoring.
Caution! Deciding whether a patient is to receive home quarantine requires careful clinical assessment of safety and health risks involved in home healthcare.
How to home quarantine for suspected infections?
- Arrange a well-ventilated single room for the patient.
- Limit the number of caretakers. It is better to designate one person who is in good health and has no chronic diseases to take care of the patient. All visits should be avoided.
- Family members of the patient should live in different rooms or at least keep more than one meter from the patient. Nursing mothers can continue to breastfeed their babies.
- Restrict the movement of the patient and minimize the shared areas between the patient and family members. Make sure that the shared areas (kitchen, bathroom, etc.) are well-ventilated by opening windows frequently.
- Wear a mask when staying in the same room with the patient. The mask should fit the face snugly. Avoid touching or adjusting the mask with unclean hands. Replace the mask immediately when it is contaminated. Wash hands after removing the mask.
- Wash hands after having any direct contact with the patient, or entering or exiting the patient’s isolation ward. Wash hands before and after preparing food, before eating, after going to the toilet, and when hands look dirty. If hands are not visibly dirty, clean them with a hand sanitizer; if hands are visibly dirty, wash them with soap and water.
- After washing hands with soap and water, it is best to use disposable paper towels to dry hands. If they are not available, wipe them with a clean and dry textile towel, and replace it when it becomes wet.
- Maintain good hygiene of the respiratory tract (wear masks, use tissues or lift your elbow to cover your mouth when coughing or sneezing, and wash hands immediately after coughing and sneezing).
- Disinfect and discard the items used to cover the nose and mouth, or wash them properly after use (such as washing handkerchiefs with soap or detergent and water).
- Avoid direct contact with human droplets, especially oral or respiratory secretions, and avoid direct contact with patient’s stool.
- Wear single-use gloves when cleaning the mouth and respiratory tract of patients as well as handling the patient’s feces and urine. Do not discard the gloves carelessly.
- Avoid direct contact with the patient or items contaminated by the patient, such as toothbrushes, tableware, food, drinks, towels, bath towels, bed sheets, etc. Wash dishes with detergent or discard them after use.
- Use ordinary household disinfectants containing diluted bleach (bleach: water = 1: 99) (most household bleaches contain 5% sodium hypochlorite) to regularly clean and disinfect the frequently-touched objects, such as bedside tables, bed frame and another bedroom furniture. Clean and disinfect bathroom and toilet surfaces at least once a day.
- Use ordinary laundry detergent and water to wash the patient’s clothing, bed sheets, bath towels, towels, etc., or wash them in a washing machine at 140-194ºF with ordinary household laundry detergent, and then dry the above items completely. Put contaminated bedding in laundry bags. Do not shake contaminated clothing to avoid direct contact with skin and your clothes.
- Wear disposable gloves and protective clothing (such as a plastic apron) before cleaning and touching clothing, bedding and surfaces of objects contaminated by human secretions. Wash hands before putting on gloves and after removing them.
- Patients should stay at home until a full recovery. Deciding whether the patient has recovered requires clinical and/or laboratory diagnosis (rRT-PCR assays should be carried out at least two times and produce negative results; the interval between two consecutive assays should be at least 24 hours).
What should I do amid a close contact with a COVID-19 patient?
Monitoring close contacts: All persons (including medical professionals) who may have been in contact with a suspected case should have a 14-day medical observation. The observation starts from the last day of contact with the patient. Seek medical help as soon as you experience any symptoms, especially fever, respiratory symptoms such as coughing, shortness of breath, or diarrhea. During the observation, contacts should keep in touch with medical professionals. Medical professionals should inform the contacts in advance, if symptoms present, where they can seek medical help, the most suggested transportation, when and where to enter a designated hospital, and what infection control measures to take.
Specific instructions are as follows:
- Notify the hospital in advance and inform them that a contact with symptoms is going to the hospital.
- Wear a surgical mask on the way to the hospital.
- Avoid taking public transportation to the hospital. Call an ambulance or use a private vehicle, and try to keep the windows open on the road.
- Close contacts of patients should maintain respiratory hygiene at all time and wash their hands frequently. Stay far away from other people (> 1 m) while standing or sitting on the road to or at the hospital.
- Contacts of patients and their caregivers should wash their hands properly.
- Any surfaces contaminated with respiratory secretions or bodily fluids on the way to the hospital should be cleaned and disinfected with ordinary household disinfectants containing diluted bleach.
How to control hospital infection?
The medical workers must strictly follow hygiene and infection control standards in healthcare facilities and the medical procedure protocols to reduce the transmission risks. They must take a better control of hospital infection by practicing good personal protection measures, hand hygiene, ward management, environmental disinfection and waste management. Pre-examination and triage office/station: wear protective work clothes, work caps, medical surgical masks, etc. Outpatient, emergency, fever outpatient and isolation ward: during daily consultations and rounds, wear protective work clothes, work caps, medical surgical masks, etc.; when contacting blood, body fluids, secretions or excreta, wear latex gloves; when performing operations/procedures that may incur aerosol or body fluid splashing such as tracheal intubation, airway care and sputum suction, wear N95 masks, facial screens, latex gloves, impermeable isolation clothing, protective clothing and respirator if necessary. The visitation control system should be strictly implemented for the patients in isolation. If it is necessary to visit a patient, the visiting personnel should be instructed for proper personal protection measures according to the relevant regulations.
Why do the medical staff of fever clinic wear protective clothing in consultations?
(1) Medical personnel are the main force of epidemic prevention and control. Only when they do well in personal protection can they help patients better.
(2) In order to ensure the health and occupational safety of medical workers so that they can detect and rescue suspected cases in time and effectively, the prevention and control measures and nosocomial infection control must be enhanced in all levels of hospitals, and the protection of medical workers should be strengthened by monitoring their health and providing care and support.